Getting pregnant with PCOS
Polycystic Ovarian Syndrome (PCOS) is a common hormonal disorder that can make it harder to conceive naturally. Around 1 in 10 women have PCOS.

Polycystic Ovarian Syndrome (PCOS) is a common hormonal disorder that can make it harder to conceive naturally. Around 1 in 10 women have PCOS1, with higher instances in communities including Aboriginal and Torres Strait Islanders. In this blog, Dr Nalini Gayer, Fertility Specialist at Adora Fertility Sydney, explains what PCOS is, the symptoms associated with PCOS, why it impacts fertility, and getting pregnant with PCOS.
What is PCOS?
PCOS – Polycystic Ovarian Syndrome – is a hormonal condition. Women with PCOS may experience irregular menstrual cycles, excess body hair, weight gain, and skin changes. However, many women have no symptoms – it is estimated around 70% of women with PCOS remain undiagnosed.
Although PCOS is a cause of infertility in women, it can be overcome, often without the need for IVF.
What causes PCOS?
The exact cause of PCOS is not known. Studies point to lifestyle, environment and genetics as the key factors. High energy, high carbohydrates, a fatty diet and lack of exercise are strongly associated with the rise in incidence of PCOS.
It has been shown that up to 80% of women with PCOS are ‘insulin resistant’, which means that their bodies don’t recognize the insulin levels produced in response to the intake of carbohydrates and therefore continue to produce insulin resulting in an excess.
These high insulin levels cause the body to produce more androgens (male sex hormones) and less oestrogens (female sex hormones), which disrupts the menstrual cycle and ovulation, making it hard to get pregnant. High androgens also lead to weight gain and excess body hair.
Despite its name, PCOS affects the whole body, not just the ovaries. Uncontrolled PCOS can lead to an increased risk of diabetes, hypertension, increased cholesterol levels and heart disease.
PCOS symptoms
PCOS symptoms vary from person to person and range in severity, making PCOS difficult to diagnose. Common symptoms include:
- Menstrual problems - irregular periods or no periods at all
- Excessive facial and body hair caused by high levels of androgens
- Weight gain
- Thinning hair and hair loss
- Acne and dark pigmentation of the skin
- Difficulty falling pregnant
If you have one or more of these symptoms, it is worth seeing your healthcare provider or a Fertility Specialist, as an early diagnosis of PCOS is important to help manage the condition.
Fertility and PCOS
PCOS can make it more challenging to fall pregnant. This can be due to:
Lack of ovulation:
Anovulation is the main reason many women with PCOS struggle to get pregnant. This is because with PCOS, the ovaries are typically enlarged with many immature follicles (fluid-filled egg sacs) around the edge, which do not mature and release an egg. These are known as ‘polycystic,’ which is how PCOS gets its name.
Irregular menstrual cycles:
Irregular cycles make it harder to track fertile days and therefore understand when you should time intercourse in order to conceive.
Growth of polyps inside the uterus:
The lack of ovulation caused by PCOS may lead to endometrial polyps, affecting embryo implantation.
Weight gain:
Some women with PCOS have a high BMI, which in itself makes it harder to conceive and also exacerbates the symptoms of PCOS.
How to get tested and diagnosed for PCOS
PCOS testing and diagnosis involves an examination of your medical history, overall health, and specific blood tests and scans. These tests may include:
- Hormonal profile blood tests including pituitary and ovarian hormones, testosterone levels, and Sex Hormone-Binding Globulin (SHBG), which controls the amount of testosterone in your blood
- Full glucose test for glucose and insulin levels and fasting insulin levels
- Pelvic ultrasound scan to examine the ovaries, antral follicular count, and endometrial thickness
- Serum lipids, including cholesterol
For a diagnosis of PCOS, other common causes of PCOS symptoms are typically ruled out first. According to new internationally recognised clinical guidelines released in 2023, to confirm PCOS women must generally have two of the following three symptoms:
- Biochemical or clinical evidence of excessive androgen levels – such as blood results that show excessive testosterone levels, or the signs of it, such as abnormal hair growth
- Ovulatory dysfunction – irregular periods or no periods at all
- Polycystic ovaries as seen on an ultrasound scan or elevated Anti-Mullerian Hormone (AMH) levels (ovarian reserve)
Getting pregnant with PCOS
Having PCOS does not mean you cannot get pregnant or that you need fertility treatment – it all depends on how PCOS affects you.
A Fertility Specialist will be able to advise the right pathway to pregnancy. Fertility Specialists are highly experienced in understanding and treating the varying effects of PCOS. They will conduct initial fertility tests, including a pelvic ultrasound scan, to accurately assess your current reproductive health and your general health, BMI, and well-being.
If your BMI is high, you may be advised to reduce it to a healthy level before trying to get pregnant, either through lifestyle and diet changes or weight loss management. If your BMI is extremely high then medication may be advised.
It is important to prevent weight gain by switching to a high protein, low carbohydrate diet maintaining portion control and combining this with regular exercise.
Your Fertility Specialist may also advise a course of medication to try to stimulate ovulation, such as Clomid or Letrozole, or Metformin, which also reduces insulin levels to help regulate your periods.
You can then use at-home ovulation prediction kits to help time intercourse for whenovulation is imminent. Ovulation prediction kits are easy and simple to use and work much like a home pregnancy test - a positive result means ovulation is likely in the next day or so. Your Fertility Specialist will advise when you should start testing for ovulation.
Fertility treatments for PCOS
If medication and weight loss do not help you to conceive, you may be advised to have a fertility treatment called Ovulation Induction (OI).
For women with PCOS, OI typically involves injections of fertility medication, such as Follicle Stimulating Hormone (FSH), which stimulates your ovaries to produce a mature egg. You will be carefully monitored throughout your OI cycle to ensure you are safely responding to stimulation. This is because women with PCOS tend to be more at risk of developing a condition called Ovarian Hyperstimulation Syndrome (OHSS), which is where the ovaries ‘over respond’ to fertility medication and produce too many mature eggs.
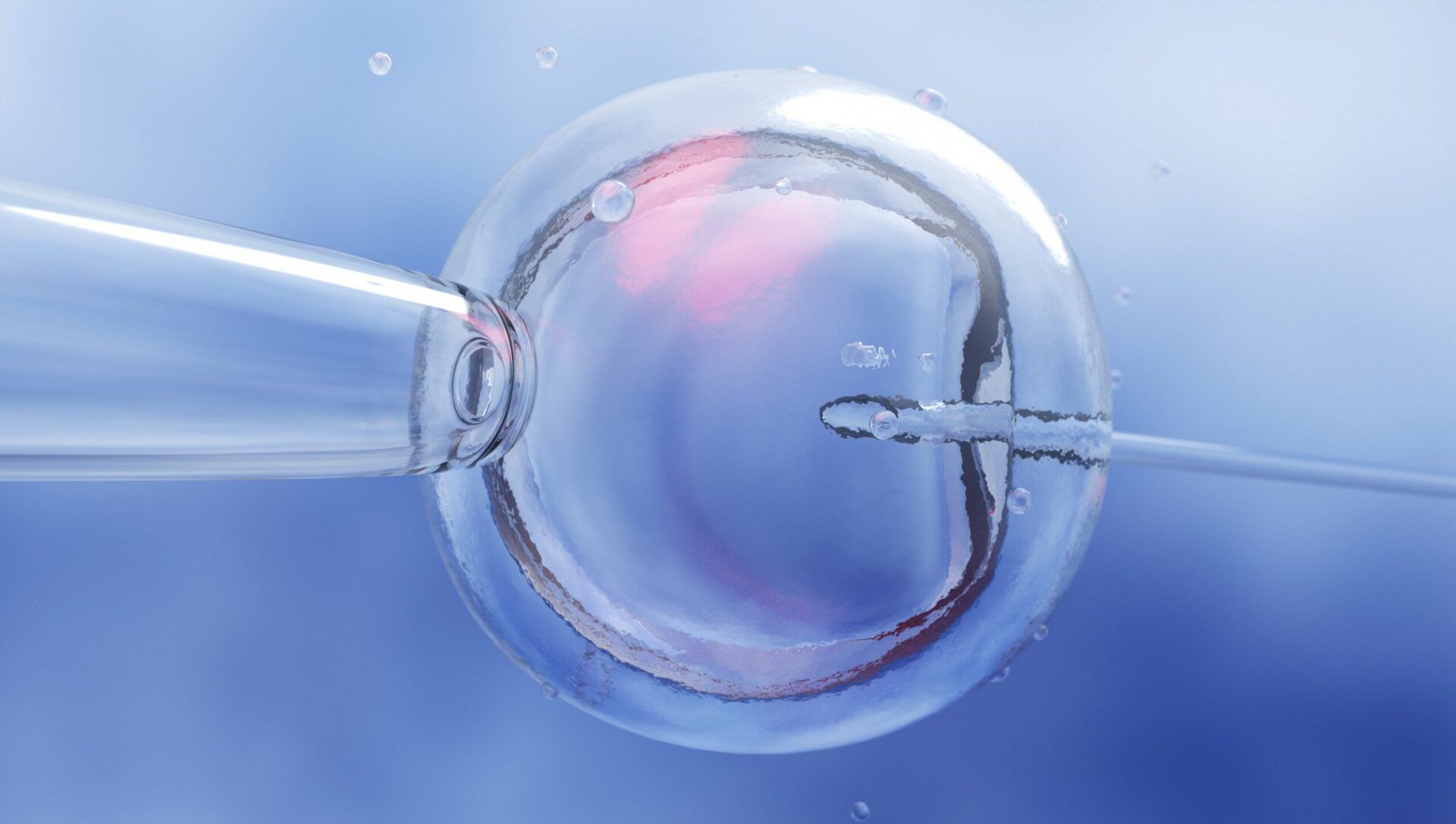
You may also be offered IVF (In-Vitro Fertilisation). IVF also involves the use of fertility medication at a carefully planned dose to ensure you produce a good number of mature eggs for your IVF cycle. Eggs are then fertilised in the laboratory with either partner sperm or donor sperm, with the best embryo transferred into your uterus.
Next steps
If you have PCOS and are trying to conceive or are worried about PCOS symptoms and your fertility, we are here to help.
At Adora Fertility, our Fertility Specialists would welcome the opportunity to discuss your situation with you. Please contact us to find out how we can help.
Sources
Related Articles

The Two Week Wait
If you are trying to conceive you will be familiar with the ‘two week wait.’ This is the stretch o...

How to increase chances of pregnancy
Planning to try for a baby? Beginning your journey or expanding your family is an exciting time. A...
What is In Vitro Fertilisation and How Does it Work?
In Vitro Fertilisation - known as IVF - was once a medical miracle. We’ve come a long way since 19...